More about minocycline
 Read with caution! This post was written during early stages of trying to understand a complex scientific problem, and we didn't get everything right. The original author no longer endorses the content of this post. It is being left online for historical reasons, but read at your own risk. |
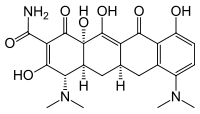
(above: minocycline)
If you read the post on tetracyclines a couple months back, you may have felt you were left hanging with regards to the effect of minocycline. In Luigi 2008, hamsters (infected intraperitoneally with 263K prions) treated (intraperitoneally, starting 1 hour after infection, at the same site) with minocycline experienced an 81% increase in survival time, compared to just 25% and 32% for tetracycline and doxycycline. Yet it was doxycycline, not minocycline, that made it to a human clinical trial in Italy. This might be because LipoDoxycycline (doxycycline trapped in lisosomes) was available for Luigi’s other experiments with intracerebral infusion of the drug, which helped to establish more evidence for efficacy. But in any case, it raises the question of why no one followed up on minocycline (spoiler: actually, someone did).
I remembered this issue when I ran across minocycline again in the Huntington’s Disease literature, in Kim 2011‘s review of proposed HD therapies. On further investigation, it turns out that minocycline has been tested for practically every neurodegenerative disease.
Noble 2009 gives a clear and concise review. Broadly speaking, there are three proposed mechanisms for minocycline’s supposed benefit in neurodegenerative disease:
- Disaggregation of amyloid fibrils and plaques
- Reduction of neuroinflammation
- Prevention of apoptosis
In support of each of these three mechanisms, Noble cites several different studies showing minocycline’s interactions with various relevant markers and factors, both in vitro and in vivo.
As documented in the history of tetracyclines post, interest in tetracyclines as antiprion agents arose from a search for structural analogs of iodoxorubixin, which was believed to interfere directly with amyloid fibril formation. The fact that Forloni 2002 showed a delay in onset in hamsters inoculated with brain homogenate that had been coincubated with tetracyclines also points to some sort of cell-free mechanism for tetracyclines inhibiting PrP conversion. So the original interest in tetracyclines-for-prion-disease grew out of mechanism #1 above.
So there are at least three broad mechamisms by which minocycline could protect against prion diseases. And Luigi’s study provides some interesting evidence that it really works in vivo, but the evidence is not as solid as that for many other proposed therapeutics at this point. Since the mice were infected peripherally and treated with minocycline immediately (1 hour after infection), the study can’t demonstrate that any therapeutic action of minocycline took place in the brain. Skeptics could dismiss minocycline as just affecting transport to the brain, the body’s peripheral response to infection, etc. and claim that it therefore wouldn’t work against sporadic or genetic prion diseases.
Minocycline does cross the BBB, at least. Noble introduces the compound as follows:
Minocycline hydrochloride… is a broad spectrum second generation semi synthetic derivative of the bacteriostatic antibiotic tetracycline. Minocycline and tetracycline share a common core of four six-membered rings, with minocycline having modifications at three sites on the conserved structure compared to tetracycline (Fig. 1). These modifications to the core structure increase its half-life in comparison to first generation tetracyclines and have improved the absorption of minocycline into the central nervous system and its penetration into cerebrospinal fluid.
But BBB penetration is only a piece of the puzzle; the drug also has to have an effect once it gets to the CNS, and not all scientists believe that minocycline has the neuroprotective effects that Noble describes. Those who do believe it have had plenty of opportunities to make their case: minocycline has already made it to human clinical trials for practically every other neurological condition you can imagine: Fragile X, ALS, regressive autism, Huntington’s, Alzheimer’s, Parkinson’s, and yet others. As far as I can tell none of these trials have concluded that minocycline had a positive effect. In the Huntington’s world, there have been reports here and there of good results in patients (e.g. Denovan-Wright 2002) but by 2010 the Huntington Study Group was pretty much ready to declare futility and call off any further studies [Huntington Study Group 2010]. HDBuzz’s first article summed up the news: “this study… is probably the end of the road for minocycline… in HD.” I haven’t bothered to look at every other disease, but everything I’ve seen is at least as negative. In ALS, Phase III trials found that minocycline significantly accelerated patients’ decline [Gordon 2007].
Decisions to enter clinical trials aren’t taken lightly– all of these diseases had to have good evidence from animal studies suggesting minocycline would work– so it does seem a bit like the universe is conspiring to trick us. Perhaps there’s something special about minocycline in mice and not in humans. Who knows.
But as far as prion diseases are concerned, it’s not even clear that minocycline even works in mice. Riemer 2008 tested minocycline delivered orally at 200 mg/kg/day starting at 100 days post infection (dpi) in C57BL/6 mice infected intracerebrally with 10-3 brain homogenate of 139A prions. Riemer found no significant difference in survival: 178±5.7 days in the treated group (n=17) vs. 175±8.4 days in the control group (n=16).
There is plenty of room for debate on what is the right time to start treatment to properly assess a drug’s efficacy. At 1 hour post infection, skeptics can argue that the therapeutic effects aren’t relevant to treating CNS infections (as discussed above), but at 100 days post infection, the infection may be too entrenched to respond to compounds that would have worked earlier and could be relevant to humans. It’s possible that a study administering minocycline starting at 14 dpi would have had better results than Riemer found. But then, minocycline has already been the source of a lot of dashed hopes for other neurodegenerative diseases. If it does get any further attention in prion mouse studies, we may need to be cautious in our interpretation of the results.