The rise and fall of pentosan polysulfate in prion disease
Next to quinacrine, pentosan polysulfate (PPS) (above) has probably been the second-most examined drug in the treatment of prion disease. PPS never made it to an official clinical trial in the United States, but Japan and the U.K. each ran clinical trials, both of which failed. PPS has since been pretty much abandoned as a potential prion treatment, for more than one reason, but we can learn a lot from the history of research into this compound as an antiprion therapeutic.
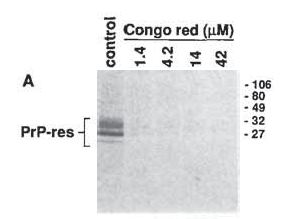
Pentosan polysulfate was tested in mouse models of prion disease as early as 1984, but the real story begins, in a way, with Caughey & Race 1992, who observed that Congo red inhibits PrP accumulation in prion-infected cell culture. Congo red was originally invented as a stain for cellulose but has for decades been used in laboratories as a stain for amyloid plaques, which, after all, earned the name “amyloid” for their misleading resemblance to starch (amylum in Latin), which is composed of the same glucose subunits as cellulose, under staining. Like Alzheimer’s and some other neurodegenerative diseases, scrapie results in the deposition of amyloid plaques in brain tissue. Since Congo red stains (read: binds to) amyloid plaques effectively, Caughey and Race wondered if it might interfere with the formation of amyloid plaques as well. And it did – in fact, it pretty much completely abolished the formation of PrP-res, as shown in Fig 1A:
But Congo red was not exactly ready for prime time as a therapeutic compound. In fact, according to Wikipedia it’s so toxic that even the textile and paper industries won’t use it anymore (always a bad sign). So Caughey and Race’s discovery touched off a search for less toxic compounds with the same PrP-res-inhibiting property.
That search led ultimately to several hits including cpd-B and curcumin. But the race had been won before it started: a year before Caughey and Race’s discovery, another group had already announced that adminstration of the polyanion compound pentosan polysulfate resulted in a massive extension of survival in scrapie-infected mice [Diringer & Ehler 1991]. In fact, without any fanfare at all, these two had reported a significant effect of pentosan polysulfate as early as 1984, in a study whose primary purpose was to evaluate the efficacy of another polyanion compound: dextran sulfate 500 [Ehler & Diringer 1984]. Predictably, the 1984 study had found that DS500 was only effective against peripheral infection and not intracerebral – “polyanions” by definition are highly charged compounds, which the BBB‘s border control agents hate. But Diringer and Ehler’s 1984 and 1991 studies evaluated PPS’s efficacy only in peripherally infected mice, and only with drug administration either prophylactically or very early in the disease course. Ladogana 1992 had likewise shown efficacy against peripheral infection for DS500, pentosan polysulfate (referred to in that study as SP54) and suramin. In fact, Ladogana even tested DS500 and suramin (but not PPS) against intracerebral infection and found a small but significant effect for DS500.
So in fact, lots of work on PPS preceded Caughey’s discovery that Congo red inhibits PrP-res formation. But I chose to start the story with that oft-cited paper because it coincided with the beginning of scientific acceptance of the protein-only hypothesis and, with it, a new perspective on what a compound needed to do in order to fight prion infection. The studies by Ladogana, Farquhar, Diringer and Ehler all took place back in the dark ages when people thought scrapie was an “unconventional virus”, so much of the discussion in these papers centers on the supposed “antiviral” properties of DS500 and PPS. By 1993, putting together the newly emerging prion hypothesis (described as “controversial”) with the results from the 1992 Congo red study, Caughey had a better idea of why PPS might have been effective: perhaps it inhibited PrP-res formation just like Congo red. PPS isn’t exceptionally similar to Congo red, but the two do have two sulfate anions in common:
Congo red
Pentosan polysulfate
And sure enough, Caughey was able to show that PPS inhibited PrP-res formation “in vivo” [Caughey & Raymond 1993], by which he actually meant ex vivo: in cell culture, not in a whole organism.
And curiously, no one provided in vivo validation of this finding for over a decade. Of course, PPS was already known to be effective in vivo – in early or prophylactic administration in peripherally infected mice. What remained was to show that PPS was also effective against intracerebral infection, and that it could abolish the amyloid plaques that characterized scrapie infection in mice and CJD in humans, plaques composed of a protein beginning to gain acceptance as being the pathological agent: PrP.
Instead, the next decade saw a series of basic science papers on PPS and related molecules such as heparin and heparan sulfate, using these molecules as tools to understand the biological and biochemical properties of PrP [Caughey 1994a, Caughey 1994b, Shyng 1995, Brimacombe 1999]. The most surprising of these was the confirmation that although PPS inhibits PrP-res formation in cell culture, it stimulates PrP-res formation in cell-free conversion [Wong 2001]. One other paper testing PPS in vivo did emerge after several years [Farquhar 1999], but it didn’t cite Caughey’s work and managed to remain wholly agnostic as to the identity of what it called the “bovine spongiform encephalopathy agent”, avoiding calling it either a ”prion” or a “virus”. Farquhar successfully duplicated the earlier in vivo results, showing that a single dose of PPS could dramatically delay disease onset or prevent it altogether, if administered intraperitoneally within several hours of the initial peripheral infection. The results replicated across several different mouse strains, but the issue of PPS’s possible interference with PrP and efficacy against CNS infections was left untouched.
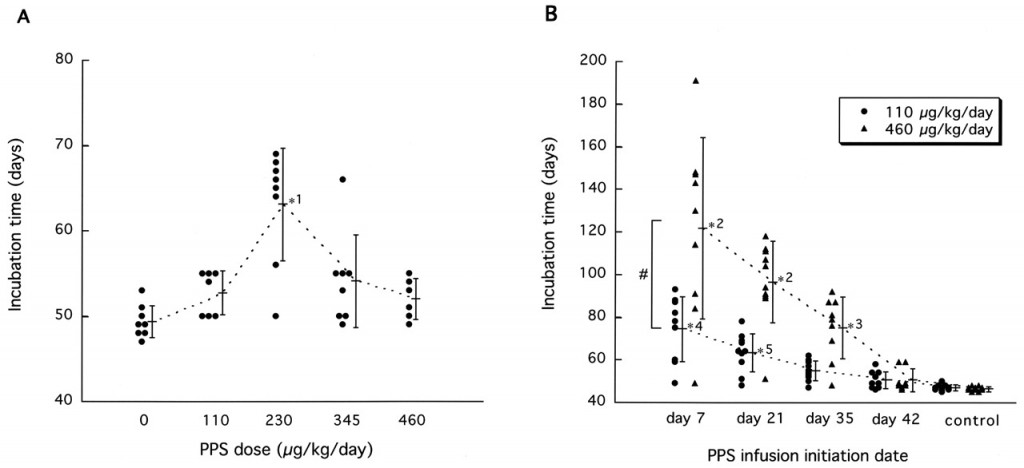
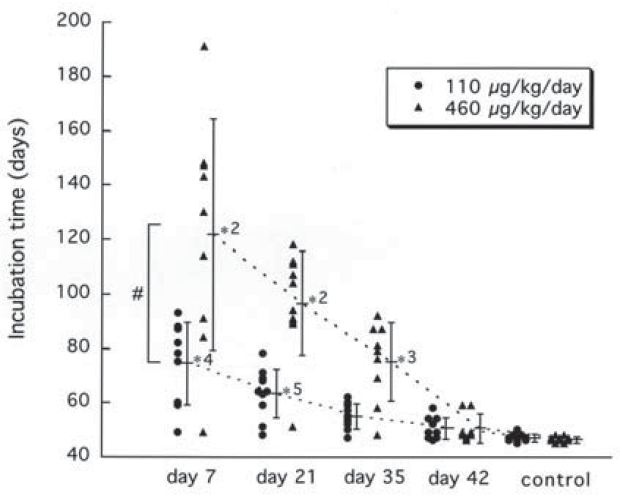
When evidence on the in vivo efficacy of PPS against CNS prion infections finally did surface after more than a decade, it did so in a spectacular fashion. In 2004, Katsumi Doh-Ura demonstrated that continuous ventricular infusion of PPS of mice could extend survival by as much as 2.4-fold [Doh-Ura 2004]. His primary model was Tg7 mice expressing hamster PrP, infected intracerebrally with 263K hamster prions. Doh-Ura tested not only PPS but also quinacrine (no effect), chloroquine (no effect), E-64d (no effect), and amphotericin B (some effect). The whole experiment was exquisitely designed to test the drugs’ efficacy against CNS infections without bumping up against issues of blood-brain barrier permeability. It must have been an impossibly difficult experiment to pull off: Doh-Ura implanted miniature devices in the backs of the mice, just under the skin, with tubes leading to their left ventricles to continuously drip tiny amounts of PPS for four weeks after implantation until the chemical ran out. And it wasn’t prophylactic, either: the mice were treated beginning at 7, 21, 35 or 42 days post-infection (dpi), meaning the surgery had to be done on already scrapie-infected mice. Perhaps this explains what one prion researcher recently told me: Doh-Ura’s result was the best result there’s ever been for prion therapeutics; it’s just that no one has managed to reproduce it.
In the published literature, at least, no one has even tried to reproduce it. That’s probably in part because of the technical difficulty involved and in part because Doh-Ura had already left no stone unturned. The incredibly thorough study varied both the dose and the date that drug administration was started, as summarized beautifully in Fig. 2:
The results are very clear: PPS is most effective at a medium dose of 230 ug/kg/day and when administered as early as possible, though it still has a significant effect when administered late in the disease. At its best, it delayed death from 51 dpi for controls to 123 dpi for mice treated with 460 ug/kg/day starting from 7 dpi.
Not satisfied to show an effect on just one model, Doh-Ura also varied the mouse model and prion strain in question. His primary experiment used Tg7 mice, which overexpress hamster PrP and no mouse PrP, infected with 263K hamster prions; subsequently he also tested PPS by the same protocol in Tga20 mice (which overexpress mouse PrP) infected with Fukuoka-1 and RML prions. Those experiments showed smaller (regression to the mean, perhaps?) but still quite large, extensions of survival – 117% and 49% respectively when treatment was begun at 14 dpi.
Doh-Ura also tried subcutaneous administration of PPS with, as would be expected, no effect: PPS could not cross the blood-brain barrier.
The study didn’t skimp on follow-up experiments to figure out how PPS had worked, either. Doh-Ura did immunohistochemistry on the treated mouse brains and found a remarkable reduction in PrP deposits. In fact, the neurodegeneration that had killed the mice was almost wholly concentrated in the right hemisphere of the brain, while the left hemisphere, where the infusion site was, was spared the worst of it. Doh-Ura also assayed the infectivity of the mouse brains in the same blunt way that it’s still done today – by injecting their brain homogenate into other mice and comparing the survival of those mice to a standard table. Last but not least, Doh-Ura did toxicology experiments on mice, rats, and dogs – again, with intraventricular infusion – to determine the tolerated dose and assess what adverse effects might be anticipated.
The overall picture was of a drug of fairly low toxicity that reduced infectivity through direct action on the infectious protein itself, largely regardless of prion strain, and could more than double the incubation time of the disease if administered early enough. It was, and probably still is, the strongest result that’s ever been shown for a potential antiprion drug. But there were two catches.
Two big catches. First, it had to be administered directly into the brain. Second, and more importantly, the study provided no evidence for – indeed, some evidence against – the idea that PPS would work in already-symptomatic animals. As shown in Fig 2B above, Doh-Ura tested PPS at 7, 21, 35, and 42 dpi in mice that showned “definite symptoms” at 49 dpi (though Doh-Ura allowed for the possibility that more subtle earlier symptoms could have gone unnoticed) and died at 51 dpi. The effect of the drug was huge at 7 dpi, small by 35 dpi, and so tiny as to be statistically insignificant by 42 dpi. To help you see this, Doh-Ura has actually drawn line segments connecting through the means of the different groups:
The the lack of a ‘day 14′ experiment to evenly space the X axis makes the lines a bit misleading (the group means aren’t actually collinear as they appear in this figure), but the trend is pretty obvious. Based on this figure you can have a pretty good guess that mice not treated until they exhibited symptoms at day 49 or day 50 would not experience any increase in survival.
And Doh-Ura fully recognized this, noting that “our data do not guarantee similar effectiveness in human patients who already have signs and symptoms of the disease”. Acknowledging this, and acknowledging as well the personal and public health risks of installing intraventricular catheters in prion dsiease patients, Doh-Ura still chose to end the paper on an optimistic note. Though the United States was yet to start its own clinical trial of quinacrine, PRION-1, Doh-Ura had read the literature on quinacrine in mice and hamsters and had (correctly) concluded that quinacrine would not prove effective in humans. So he put forth PPS as the next candidate for clinical trials:
As an immediately applicable remedy, however, continuous intraventricular PPS administration with an infusion device may be a candidate for a clinical trial, with a view to preventing the disease in those people categorized as being at extremely high risk or to improving the prognosis of diseased people with TSEs.
PPS was already approved in the U.S. (and presumably in Japan too, though I can’t find any confirmation of that online) for interstitial cystitis, a.k.a. painful bladder syndrome, which is basically a diagnosis of exclusion meaning “we can’t identify any other problem to explain your symptoms, so we’ll call it this”. For a review of pentosan polysulfate in painful bladder syndrome, see Teichman 2002. The bladder connection seems at first interesting in light of the known connections between prion disease and bladder problems (see posts on dapsone and ibuprofen), though it’s almost surely a coincidence. In any event, here you have an already approved drug which might be effective against a sudden, deadly disease with no known treatment or cure. Almost immediately, neurologists started trying PPS in their prion disease patients.
Over the next five years, ambiguous reports of human results trickled in from several places. In the peer-reviewed journals, a handful of case reports arrived, some of which reported considerably extended survival [Todd 2005, Parry 2007, Rainov 2007] and some of which did not [Whittle 2006], though in no case was the patient’s condition seen to actually improve.
Other reports came from outside the traditional journal setting. A series of short articles in BMJ [Dyer 2003, Gould 2003, Mayor 2003] and a subsequent BBC report documented one family’s battle to get PPS (which is not an approved drug in Britain) approved for their son Jonathan Simms – they eventually prevailed and the young man, though still sick, remained alive with vCJD for 10 years (he passed away in 2011) while being treated with PPS – possibly the same patient from Todd 2005. BBC also reported that MRC had announced the drug “had appeared to help several people live longer than expected.” And in a powerpoint apparently presented at a meeting in Glasgow organized by CJD Alliance, Dr. Ian Bone reported on eight U.K. patients who had, again, lived slightly longer than expected, though with multiple complications related to the ventricular catheters and one possible adverse reaction to the drug itself [Bone 2006].
That powerpoint is actually a more accessible discussion of the issues involved in the study design than many of the published papers are. Bullets on slides 2 and 23 show a key part of Bone’s thought process: there are too few prion disease patients, and their diseases are too urgent, for there to ever be a large, statistically powered case/control study as is the standard in medicine. Instead, we are stuck with an observational study of a handful of patients – but if we can use a “surrogate marker” to assess disease progression, maybe we can tell if the drug is working in each individual. It is this same thought process that motivates our early biomarkers research goal at Prion Alliance.
Formal reports on PPS’s efficacy finally came out in 2008-9. Bone reported that the seven patients formally included in the observational study in the U.K. had indeed lived longer than the mean for their respective prion diseases, but clinical symptoms as well as MRI – his “surrogate marker” – both showed continued disease progression after drug treatment began [Bone 2008]. The slightly longer survival might be due to PPS but Bone felt he couldn’t rule out several other possible explanations:
chance alone and biases such as lead-time bias from attentive carers diagnosing onset early; selection bias from included patients having prolonged survival whilst awaiting PPS or bias from increased use of active interventions for complications in more actively managed PPS patients amongst others
The report doesn’t take a firm stance for or against continued use of PPS in humans, instead concluding that “More experimental work in animal models is clearly needed” and that “Until then, all patients with prion diseases considering PPS therapy should be informed of existing evidence and, if opting for treatment, managed and monitored in a standardized manner”.
The following year, Doh-Ura and his colleagues reported on their use of PPS in eleven patients in Japan [Tsuboi 2009] with almost identical results. Again, the patients survived longer than mean for their diseases, but not out of the plausible range, and showed “continued deterioration” after drug treatment commenced.
Both of these formal reports discuss the possibility that different doses might be more effective, and neither rules out the possibility of further use of PPS. But not much has been published on PPS since then: a Google scholar search for more recent papers on prion pentosan polysulfate since 2011 turned up only one more case report [Terada 2010] and a good review of all the human case reports and observational studies [Appleby 2011].
In reading all these reports, perhaps the most interesting thing I noticed was in Bone’s Table 1 introducing the seven patients from the U.K. observational study, including their dates of disease onset and treatment and their clinical state [Bone 2008]. The patients had started PPS treatment anywhere from 6 months to 2.5 years after disease onset. At the time that the official observational period commenced (which was for most patients 1-2 years after they had already begun receiving PPS), three were bed-bound and two were chair-bound.
We don’t know whether the patients were already bed-bound or chair-bound when they started PPS treatment, but given the length of time between disease onset and treatment, it does seem likely that they were very sick by the time they started receiving the drug.
In the mouse study that touched off all this interest in PPS, Doh-Ura stated that the first noted symptom in the mice was “ambiguous signs of reduced activity” two days prior to death, so on average 49 dpi, while his experiments showed no significant effect of PPS even when started at 42 dpi. Since investigators won’t notice subtle symptoms in a mouse, it is very hard to know what day post infection in a mouse corresponds to the moment, in a human patient, that a diagnosis would be made. But given the disease state of the patients and the length of time between disease onset and initiation of treatment, it seems they were much closer to the equivalent of 49 dpi than they were to 35 dpi (the latest treatment date for which Doh-Ura observed a significant effect), by the time they received treatment.
Some of the delay in starting treatment for these patients was surely due to the experimental nature of the PPS treatment. But given the swift and unexpected nature of prion diseases, it seems that even under the best of conditions, it is very likely that patients will decline severely before any treatment can be started. Patients will need to exhibit a significant decline before it even triggers a hospital visit, referrals to specialists at tertiary care facilities will have to be made, and diagnosis will not always be quick or easy and tests will not always give immediate confirmation. The only exception to this rule is the handful of genetic prion disease carriers who have chosen to be tested and know their status – but healthy asymptomatic individuals will never go in for intraventricular catheterization.
Hence the inherent contradiction in pentosan polysulfate: it’s only effective at times when the patient’s condition is not desperate enough to merit such drastic measures.
Possibly this all could have been recognized at the outset: Doh-Ura’s study was extremely thorough and extremely honest about the fact that PPS required intraventricular infusion and didn’t work late in the disease. But given the complete fatality of prion diseases and the utter lack of any treatments, desperation gave way, and the story of Jonathan Simms as documented by BBC and BMJ shows that even when medical authorities are duly skeptical of a potential treatment, families will actively campaign to be able to use it. After all, they’ve got nothing to lose.