Why we recommend 23andMe to everyone we know
‘Knowledge is power’ is a trite but accurate characterization of our new outlook since December 2011, when Sonia and I embarked on a quest to cure prion diseases after she tested positive for the mutation that causes fatal familial insomnia. It may seem counterintuitive that after the one piece of genetic information we had ever received was life-changingly devastating, we could possibly be eager for even more genetic information. But when 23andMe dropped its price to $99, we jumped on it. I choose to summarize my view in the following graphic:
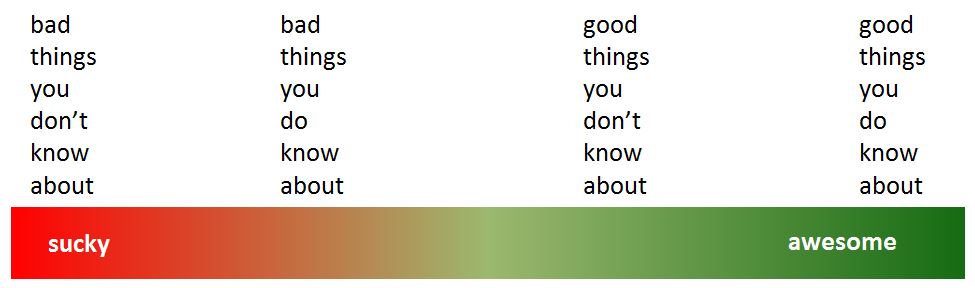
As expected, bad things suck more than good things. But for all types of things, knowing is better than not knowing.
And there are a lot of things you can come to know through 23andMe, for the astonishingly low price of $99 and only the trouble of spitting into a tube and mailing it to California. 23andMe uses a SNP chip technology to genotype about 900,000 locations in your genome. That’s not your whole genome, but it’s a lot of information – more, indeed, than anyone knows what to do with.
Working in computational genomics in Boston, I occasionally meet scientists who are all, “A million bases of DNA isn’t awesome. You know what’s awesome? 3 billion bases.” I kind of disagree – I think a million SNPs is awesome, and sequencing all 3 billion bases of your genome, though slightly awesomer, doesn’t resonate for me yet in terms of cost-benefit analysis. The cheapest price I have heard quoted lately for whole genome sequencing is $3000 at Shenzhen BGI, though that’s not a direct-to-consumer option. At MIT’s The Future of the Personal Genome forum last year, George Church told the audience that deep whole-genome sequencing was already a good deal: “If you can’t save $4,000 over your lifetime in health care costs by creatively using your genome, you, pardon me, don’t belong at the MIT forum here.” Ouch! But to me, with the price expected to continue dropping for the forseeable future, the question is more one of how much marginal benefit you can get in just the next few years for the marginal price of going whole genome now as opposed to waiting for a lower price point.
I would argue that the marginal benefit is not much. Even for the 900,000 SNPs that 23andMe genotypes, science can only offer confident and meaningful health interpretations about 10,000 or 20,000 of them at most. (The national genome-wide association study catalog has ~10,000 SNPs associated with common traits or diseases right now, but many are not yet validated or widely accepted, and the OMIM database has ~17,000 SNPs associated with rare, Mendelian diseases). The rest of the SNPs are there mostly to cover the genome – they contribute to ancestry, relative finding, and allow 23andMe’s researchers to discover new trait associations in the future.
And indeed, one thing that makes 23andMe awesome is its comprehensiveness. There are other specialized genetic testing companies just for genealogy and ancestry (Genetic Genealogy, National Geographic’s Genographic Project, Family Tree DNA), or just for carrier screening (Counsyl, Natera). I haven’t tried any of these and can’t speak to how good they might be; from browsing their websites they do offer a bit more in their respective areas of specialty, but 23andMe has pretty good coverage of all these bases – and many more.
Health
The thing you may be most eager to learn about is whether your genome has any health risks in store for you. It does. Last I checked, 23andMe had health interpretations for about 260 diseases and conditions, and the average frequency of the risk allele in disease-associated SNPs is about 38%. To a very rough approximation, your odds of not having elevated risk for anything are about .382*260 = 3E-19, also known as “just plain not going to happen.” Be mentally prepared to learn about several things you have elevated risk for, and (here’s the good news) several things you have reduced risk for. But odds are most or all of these will be only slightly elevated risks – say, 10% more risk than the average person, and that’s even less of a big deal when you consider that many of the diseases are themselves rare. If a disease has .1% incidence and you’re at 10% elevated risk, that means your chances of getting it ever are .11%.
Although most or all of the health risks you will learn about from 23andMe are small enough that you shouldn’t live your life in fear of them, you can and should respond to them. Last time I saw my primary care physician, I chatted her up about this as sort of an n = 1 survey of how the mainstream health care world views genomics (much more about this encounter towards the end of this post). She was deeply skeptical of the value of knowing your health risks, because, she said, all of the ‘what you can do’ recommendations are exactly what she always tells people to do anyway.
On reflection, I can see how as a physician who is constantly, and for the most part futilely, encouraging patients to eat healthy, exercise and get a colonoscopy after age 50, it might not seem very useful to have genetic information that for the most part carries no more specific recommendations than these. But I feel that the patient’s perspective is different than the physician’s: people may have told you for years that wearing sunscreen is a generally good idea, but knowing that you’re at increased genetic risk for melanoma might finally be the motivation to actually do it.
While you’re guaranteed to find out some relatively minor health risks, some percentage of people who do genetic testing find out about a really serious health risk. Not everyone wants to know these, and 23andMe actually gives special treatment to three issues – several SNPs associated with Parkinson’s risk; the APOE alleles associated with late-onset Alzheimer’s risk; and the BRCA1 & BRCA2 mutations that vastly elevate risk of breast cancer. To see your results you have to click through a lock icon and read some text reminding you that you don’t have to see these results if you don’t want to, and that genetic testing isn’t perfect and you should talk to your doctor and so on. But to me, the most serious information is the most important information. Knowing that you have a BRCA mutation presents you with some tough choices (see this and this from the New York Times) but can save your life. It is eminently actionable bad news. Your options aren’t quite as strong for the other two, though the peer-reviewed science does suggest that exercise reduces Alzheimer’s risk for APOE E4 carriers [Head 2012; see also NYT coverage] and that coffee reduces Parkinson’s risk at least for people with a certain genotype [Hamza 2011].
Given the care that 23andMe put into presenting these three issues, I was awfully curious how they would confront us with the information that Sonia has the mutation that causes fatal familial insomnia. They didn’t. For reasons explored in this post, it is difficult to accurately determine someone’s genotype for a very, very rare SNP, and the PRNP D178N mutation that causes fatal familial insomnia is nothing if not very, very rare. When we went into Sonia’s raw data that SNP was ‘no call’ and nothing in her health report indicated she might have this disease.
So don’t expect that 23andMe will definitively tell you whether you have a rare genetic disease. If you think Bayesianly, screening people for rare diseases is a dodgy business – the FFI mutation is one in a million, so even if your error rate is as low as one in a million, 50% of the time that you tell someone they have the mutation you’ll be wrong. And that’s kind of a big deal. So although it was disappointing not to see this SNP called correctly, I can’t blame 23andMe for being extremely cautious in interpreting people’s results.
Carrier status
Distinct from health risks, the ‘carrier status’ section refers to things that don’t affect you, but could affect your kids. If you and your would-be partner in child-having are both heterozygous carriers of a recessive disease, there is a 25% chance your child will have the disease. Cystic fibrosis, canavan disease, Tay-Sachs, and so on. Most of these are (relatively) prevalent in a particular population or ethnic group and vanishingly rare elsewhere. Since Sonia is South Asian and I’m white, it’s pretty unlikely we would happen to carry the same recessive disease, but it’s always good to check. After all, unlike your own genetic health risks, which will for the most part be very minor, these recessive diseases will be a really big deal if you do pass one on to your child. 23andMe tests for about 50 of these. Counsyl, which specializes in this area, tests for over 100.
Drug response & traits
You also get information on how you’re predicted to respond to some drugs, and various physical and mental traits about yourself. The traits won’t hold too many surprises – odds are 23andMe will correctly guess your eye color and whether your face turns bright red when you drink, and so on. About 1% of people of European ancestry will learn they’re resistant to HIV-1 because both copies of their CCR5 gene are disabled (CCR5 is a receptor that HIV-1 needs in order to enter your CD4+ cells). The drug response info didn’t do anything for me, but it could be useful, I suppose – I hear that dose-finding for people on Coumadin can be a challenge, so knowing you are genetically disposed toward a strong or weak response to Coumadin could be useful information.
Ancestry
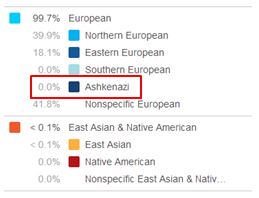
For my entire adult life, whenever I’m doing something not-very-Jewish like celebrating Christmas, people will be like “oh, but you’re Jewish, right?” Or, I’ll know someone for years and then find out they just assumed I was Jewish. I’ve never known of myself having any Jewish ancestry at all, but when this happens to you enough times, eventually you start to wonder: maybe I am a Jew. After all, most of the people asking/assuming were Jews, and I figure they know better than anyone, so eventually I felt obligated to give people answers like “maybe one sixteenth.” Nope:
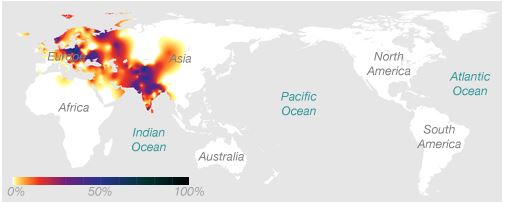
I was also surprised to learn that my Y chromosome, while common in Eastern Europe where my ancestors came from, is also quite common in North India:
And there is a relative finder which I haven’t done too much with just yet but it does seem to have some fourth and fifth cousins in store for me.
Concluding remarks
In my case, I didn’t learn anything too shocking from 23andMe – a few minor health risks I’ll be more careful about, a few minor health risks I’m relieved to not have, an assortment of interesting trait and ancestry information. But in terms of health risks, you don’t do genetic testing because it’s going to be fun and awesome, nor because you’re likely to find something directly relevant to every day of your life. At that same MIT forum I mentioned above, George Church had another memorable line, comparing genomic information to fire insurance. Fire insurance isn’t something you want to whip out and use all the time, but it’s a good idea to have it. He raised the example of hypertrophic cardiomyopathy, a condition which can cause sudden fatal heart attacks in young, fit, apparently healthy people. If you are genetically predisposed to it, you need to know that, and take appropriate action (Mayo Clinic recommends not doing competitive sports).
The fire insurance analogy is a good one. Your genome might have some deeply uncomfortable but actionable information like a BRCA mutation or hypertrophic cardiomyopathy, and it won’t be fun, but it might save your life. It’s good to go into viewing your results with an attitude of solemn caution. That’s something I forgot to do – I figured there is almost no chance they could tell me something worse than what I already know – but it is definitely the right attitude.
Once you’ve gotten through the potentially hard stuff, the rest is fun to explore. How often in adulthood do you get to learn some new facts about yourself? Whenever I see people who I know but don’t see very often (say, old classmates) I am always looking for some bright topic of conversation to avoid the old “how is work, are you still living in the same place, have you talked to anyone else we both know lately” rigmarole. In these scenarios, 23andMe has proven to be solid gold. Even people who are slightly sketched out by the idea of their own genome are fascinated by mine, and I in turn am fascinated by their reactions. The recently married couples who exchange knowing glances when I mention carrier screening – “honey, we should definitely do this”; the dudes who feel inexplicably lucky and are ready to bet $50, apropos nothing, that they’ll be resistant to HIV; the cautious souls who listen very carefully, interested but scared, and need to sleep on it to know whether all this is something they want to know.
I’ll admit that I’m a bit of an outlier – this blog is proof that I consider basically all information to be actionable information. Those who aren’t as relentlessly optimistic as me may be right to worry that they’d learn something that would make them miserable, yet about which they could do nothing. But even if you’re not going to embark on a lifelong rare-disease-curing quest, there is plenty of health information in your genome that you can do something about.
There are some detractors of direct-to-consumer genetic testing who don’t necessarily disagree with me on the value of prevention through genomics, they just disagree that people should buy the test themselves rather than getting it through their doctor. ”It’s all well and good for us as scientists,” someone told me recently, “but if you’re just some random person getting your results…”
Actually, I was just some random person getting Sonia’s genetic test results back in December 2011. It sucked. It’s true. But I’m glad I know. When Sonia was tested for FFI (by Sanger sequencing at Case Western’s prion lab), we did go through a genetic counselor, and on the whole I think I’m glad we did, though we wanted privacy at the time and probably would have gotten tested outside the medical system if we had known of an option for doing so. Shortly after getting our results we became the victims of a HIPAA violation – yes, even hospitals make mistakes, which is why I’m not too keen on the argument that you shouldn’t do 23andMe just because it’s not covered by HIPAA. Yes, the right doctor can put things in perspective and give you bonafide medical advice that 23andMe can’t, but don’t forget that a lot of people feel a deep and, in some cases very well-earned, mistrust of the health care system. I can see a lot of advantages to getting genomic information through a doctor, but I also feel that your genome is more fundamentally yours than just about anything, and no law should come between you and it – that’s why I’m not so fond of Maryland and New York’s regulations which make it impossible and difficult, respectively, to do direct-to-consumer genetic testing.
Also, who said that getting genomic information through your doctor was even an option? When I last saw my primary care physician I asked, out of curiosity, whether there was any sort of genome-wide genotyping I could get done through her and that we could discuss together. The short answer was no. She said that if I had particular reason to be concerned about a particular genetic mutation, she could refer me to a genetic counselor who could send away for targeted testing. She added that, depending on my reasons for wanting the test, it might or might not be covered by insurance and could cost $2000.
My PCP went a bit further, saying that even for BRCA mutations, she doesn’t feel that the decision to recommend testing to patients is straightforward, because knowing that you carry a mutation can keep you from getting health or life insurance down the road.
Actually, in the U.S., the Genetic Information Nondiscrimination Act (GINA) prohibits health insurance providers from discriminating against you based on your genetic information (though admittedly laws are no guarantee that discrimination doesn’t happen), and by next year Obamacare will prohibit discrimination based on all pre-existing conditions. In fact, in Massachusetts, where I live, Romneycare has already guaranteed health insurance to everybody for several years. My PCP is right, though, that there is no similar law for life insurance or long-term care or disability insurance. If you find out that you have a BRCA mutation, that could indeed keep you from getting life insurance. That sucks. But I am aghast with horrified disbelief every time I hear someone suggest that you might want to not learn something that could keep you from dying, just to make sure you spouse will get money when you do die. Let’s do some priority checking here.
Interesting aside: in 2011 in Massachusetts a Genetic Bill of Rights was proposed which would have, among other things, basically extended GINA-like protections to life, long-term care and disability insurance. It looks like it hasn’t passed yet:
@cureffi I don't, I'm sorry. I'm not sure if it has been re-introduced in the current session. I am fairly certain that it has not passed. — Dan Vorhaus (@genomicslawyer) March 11, 2013
But it does seem like the kind of thing Massachusetts would do first, so don’t rule it out in the longer term.
As you can see from my conversation with my primary care physician (n = 1), making medical sense of your genome is far from straightforward. Across the world, at conferences, on Twitter and on blogs, scientists and doctors are debating the proper place of the genome in health care. I have little to add to that debate except for my personal experience. During the two months we awaited Sonia’s genetic test results for fatal familial insomnia, we had no idea what we would do if she came up positive. Time had stopped for us. There was nothing to do but try to breathe deeply and hope. When we got her results, time came unstuck. Within a few days we had decided to throw all chips on the table in an all-out battle to cure prion diseases. Now we have this blog, and our non-profit, our new careers as scientists, and a newfound sense of purpose, satisfaction and happiness. All of which is a total surprise to us. Until you get the information, your genome is DKDK: stuff you don’t know you don’t know.
Odds are, and I sincerely hope, that your genome is much more boring than Sonia’s and that 23andMe doesn’t tell you anything worthy of your embarking on a quest. And there is plenty they can’t tell you anyway. As mentioned above, they have trouble calling really rare variants even when the SNPs are present on their chip; plenty of other rare variants aren’t even on the chip; they can’t tell you anything about repeat expansions, chromosomal rearrangements or many other sorts of genomic variation. And even for the SNPs they do genotype, science is only beginning to be able to assign any meaningful health implications to a few of them. I expect all of this to improve dramatically over time. But for $99, why wait? Already, you could learn something that will save your life. At the very least, it will make for some really good conversation.
Reminder: CureFFI.org does not provide medical nor legal advice.
