All the non-human primate studies
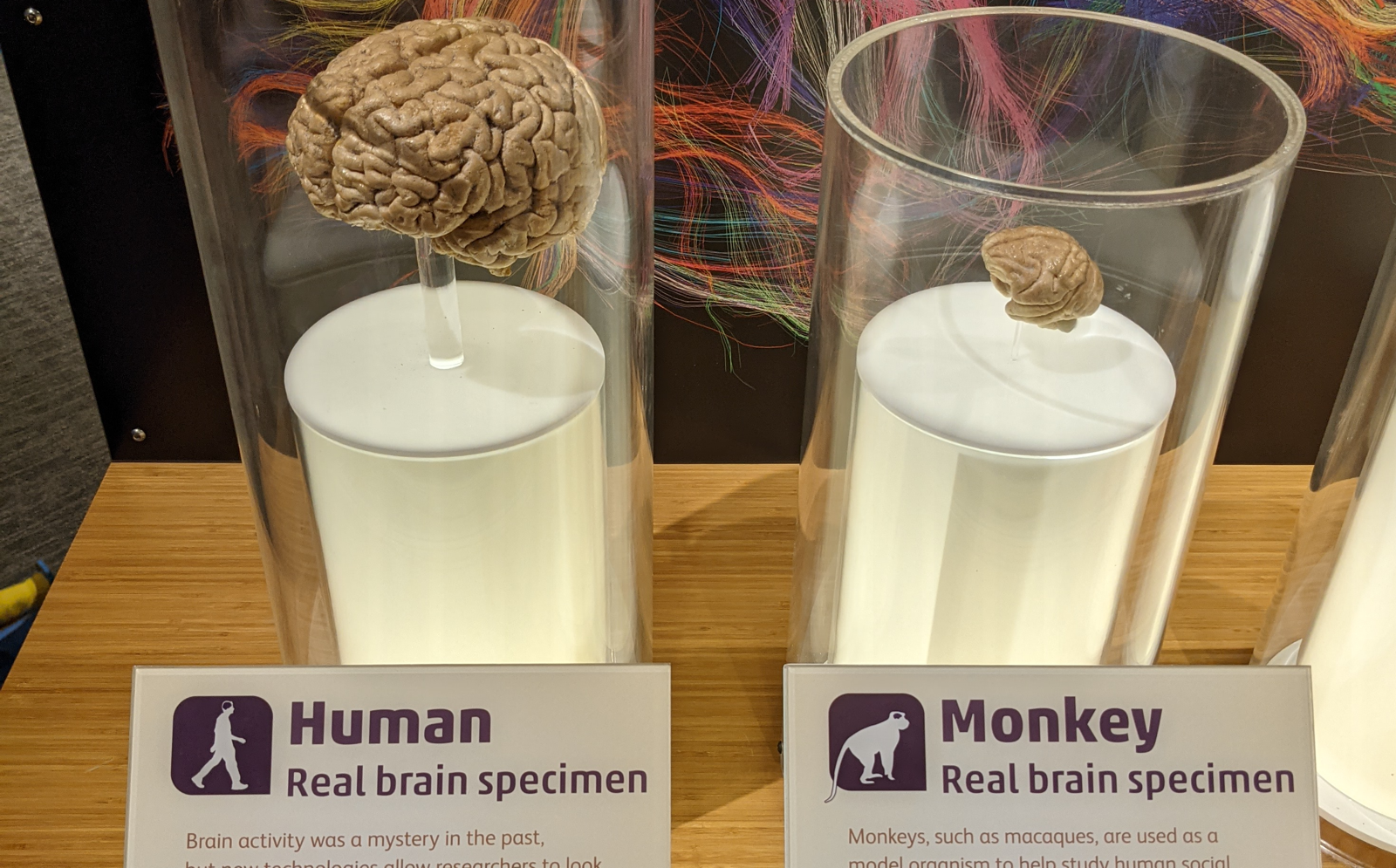
Above: actual specimens of human brain (left) and macaque brain (right), on display at the Museum of Science in Boston.
If you’ve followed this blog for the past couple years, you know that Sonia and I advocate for a preventive strategy in clinical trials of prion disease drugs. We’ve met with FDA scientists about the idea of Accelerated Approval based on a demonstration that a drug lowers PrP (measured in spinal fluid) in healthy, asymptomatic people at high genetic risk. The folks we met with at FDA were super supportive: they agreed with our case for prevention, they agreed we’re not going to randomize people to disease onset, and they agreed that PrP is so obviously central to prion disease that showing you’d lowered it could be a surrogate endpoint. But in order for PrP as a biomarker to serve the primary endpoint in a trial leading to approval, the bar for everything else has to be very high — the biomarker assay has to work really well, the drug’s safety profile has to look quite good, and the evidence from animal studies linking the drug to the biomarker to the ultimate disease outcome has to be really strong.
What exactly do those animal studies need to consist of? This point generated a lot of discussion. FDA actually has a pathway, the Animal Rule, for drugs where it’s impossible to do human studies at all. Recent examples include antidotes to nerve gas, anthrax, and plague — things where no one today actually has the condition the drug is intended to treat, but you sure as heck don’t want to wait until they do before you develop a drug for it. A drug for prevention of genetic prion disease wouldn’t go through the Animal Rule pathway, because there would indeed be human clinical trials, just with a biomarker readout rather than a direct clinical endpoint. Still, the Animal Rule guidance might provide some insight as to what bar animal studies would need to clear. As is typical of FDA guidance, there are high-level guiding principles, paired with a lot of flexibility in exactly how the science of the specific indication, specific target, and specific drug align with those principles. But at a glance, it’s clear that the bar can be fairly high. As one example: the evidence supporting approval of raxibacumab for anthrax included studies in both rabbits and monkeys, with blinding and randomization just like in a human trial, with Good Laboratory Practices documentation and pre-specified endpoints and statistical analyses [Migone 2009].
All of which raises the question: would there need to be an efficacy study in prion-infected non-human primates (NHPs)? Of course, the standard in commercial drug development these days is that pharmaceutical companies do test most new drugs in safety and pharmacology studies in primates, usually macaques, before they conduct first-in-human dosing. While such studies are certainly daunting in terms of expense and complexity,they do follow a fairly standard formula and there are commercial labs that do this routinely. But to do an efficacy study in prion-infected primates would be a different beast entirely.
How different of a beast? We realized we needed to do some homework to find out. People have been studying prion disease in primates for more than half a century, but at a glance, it was not obvious to us what — if any — combination of species, prion strain, and other variables would constitute a “model” remotely tractable for doing a drug efficacy study. Sonia decided it was time to get rigorous, and designed a systematic literature search. The vision wasn’t to review the literature per se, by which I mean, the unit of analysis was not “here’s a paper, here’s what it found” — rather the goal was to extract all the data ever reported for survival or disease onset in non-human primates infected with prions and aggregate it into one big database.
Our paper describing the findings was just published [Mortberg 2022]. After sifting through a whopping 344 papers published from 1965 to 2022, we identified 76 articles that contained data on one or more NHPs that researchers had infected with prions, yielding a total of 883 animals. The vast majority of these studies did not even remotely map onto an experimental paradigm that anyone would ever use for a drug efficacy study. In many cases, the goal of the study was to determine whether something was a potential risk to humans. So people would take a prion strain such as BSE in cattle, or CWD in deer/elk, or they would take a non-brain tissue such as blood, or they would expose animals by a non-brain route such as intravenous, and the goal was just to see if this would transmit disease. Often, the answer was either “no” or “sometimes, after a very long time”. In all, about half the animals in studies we included never developed prion disease. (The patience of our colleagues in the prion field who conduct these studies is truly incredible!) Other times, a study was a one-off, a single animal injected with some particular prion isolate, say from a single patient, and so you only got an “N of 1” survival time and no information about how variable that survival time would have been between animals. And so on. Once you whittle it down to cohorts where you had at least three animals of the same species, exposed to the exact same source of prions, by the exact same route, and successfully followed to a disease endpoint, the universe shrinks a lot. We found 39 such cohorts of animals. Some of them had huge variability in when animals got sick, and some took four or five years. If even your untreated animals take 5±1 years to develop disease, showing that a drug delays this process even further would be impossible.
There actually are, however, cohorts reported out there where both the mean and the standard deviation of the incubation time are low. As one example, the fourth passage of kuru prions into tamarins (Saguinus sp., back then called “marmosets”) in [Peterson 1978] resulted in an incubation time of 8.4±1.4 months. If one considers those numbers alone, that’s arguably not a worse “model” than humanized mice, other than being a vastly more challenging species to work with. But one catch, a big catch, is how certain can we be of getting that same result again? To the extent that the same or similar experimental paradigms (same species, same prion strain/subtype, same route of administration) were studied in more than one cohort of animals, we found that often the “second best” paradigm looked a lot less rosy than the “best case” scenario. In some cases, either luck or specific properties of the exact prion isolate used may have contributed to the short, consistent incubation time observed in one study. Luck aside, is that exact sample of fourth passage kuru from 1978 still in a -80°C freezer somewhere? And if your answer is yes, and the marker labeling the plastic tube hasn’t worn off, would you bet several million dollars and years of wall time that thawing it out and injecting it into 10 tamarins today would yield the same result as that reported in 1978? As much as drug development is inherently a risky industry, people in the industry are actually quite risk averse, and I bet you there is just no way anyone who possesses the requisite millions of dollars is going to plow those dollars straight into a large, long, complex, drug efficacy study based on a paper from 44 years ago. Instead, they would probably say, first, we’ll do a pilot study to see if the model behaves the way we think it does, we’ll do a comprehensive histology analysis to validate the model and make sure that study will give us all the data we’d need, then we’ll launch the actual study. Once you factor in the lead-in time for contracting and scheduling and obtaining animals, the variability in incubation times between animals, the tissue analysis, running a pilot followed by a “real” study, and the fact that the goal of the “real” study is to follow drug-treated animal that live longer than the baseline, you’re talking about years and years of effort. It would be a monumental undertaking carrying a lot of technical and logistic risk, and it could end up running so long that it ends up delaying patient access to a potentially lifesaving drug, exacerbating the very problem it was supposed to solve.
Therefore we should also ask: what would one gain, and what would one lose, by doing an efficacy study in such a paradigm? Framed differently: what are the advantages that an efficacy study in an NHP could provide, and how well do do the models with relatively low and consistent incubation times honor those advantages? When we went through the checkboxes one by one, we found that all the advantages for which one might look to a primate model, could probably be achieved through other experimental paradigms.
Let’s take for example one oft-touted advantage of NHPs: their big brains. As you see at the top of this blog post, even a cynomolgus macaque brain is just a tiny fraction of the size of a human brain, about 5% by mass. And macaques aren’t actually a very tractable model for prion dsiease. The monkeys with shorter and tighter incubation times have yet smaller brains. So if, say, drug distribution across a large brain is a concern, that concern could be addressed (to the extent possible in a brain that is just 5% as big) through those standard pharmacology studies in uninfected macaques. If needed, one could also bring in sheep and other farm animals, which have larger brains than some of the monkeys considered here.
Another advantage one might consider is if an NHP allowed you to study a drug’s efficacy human prion strains, rather than rodent prion strains. But for a drug where you know the mechanism of action (say, PrP lowering), this should be less of an unknown. Anyway, while it would be great to minimize all animal work with human prions for biosafety reasons, human prion strains can, after all, be modeled in humanized mice. And then you’re studying the original human prion strain of interest, without the experimental confounders of species barriers, passage numbers, and strains that may no longer be clinically relevant (such as kuru).
Another potential advantage would be if you could study the actual drug that would go into humans, rather than a “surrogate” drug made for rodents. (You’ll recall that in our published studies of antisense oligonucleotides, we used a surrogate compound targeted to the mouse RNA sequence.) But here too, you could just test that human drug in humanized mice. Insisting instead on testing it in NHPs means you end up very constrained by sequence similarity. Sure, a lot of NHPs have DNA sequences that are 90% similar to humans in the aggregate, but that 90% is per DNA base. If you’re talking about an oligonucleotide therapeutic that is 20 bases long, and requires an exact match, then only 0.9^20 = 12% of possible sequences will match. That’s just a back of the envelope to illustrate the principle, but we did the actual calculation by tiling the actual PRNP sequences for each species, and the answer was that anywhere from 2.4% to 33.8% of possible 20-base oligonucleotides targeting human PRNP would match, depending which species. When the whole battle is to find the best possible drug, throwing out anywhere from two-thirds to 98% of possible drug candidates from the starting line just based on species similarity, would be a huge loss.
All told, no NHP model seems to check all the boxes. Meanwhile, no box can be checked only by a prion-infected NHP model. While a drug efficacy study in prion-infected NHPs might not be technically impossible, the tradeoffs and sacrifices required appear to us to outweigh the potential benefits. Instead of trying to address every question in one huge, risky experiment, one might try to answer each question — drug distribution throughout the brain, mechanism of action and relevance across prion strains, potency and tolerability of human drug compound, and so on — in an appropriate model for each.
