Chlorpromazine: another prion therapeutic of yesteryear
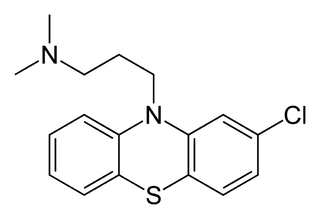
Of the four proposed antiprion compounds that have been used in symptomatic prion disease patients to date (none of which appear to have worked), chlorpromazine (above) has probably gotten the least attention. For the record, the other three are: quinacrine, pentosan polysulfate and doxycycline (and if I’ve missed any, please leave a comment to let me know).
Chlorpromazine is a phenothiazine compound, a name which refers to the fact that it is phenolic (it has aromatic rings, though technically it does not have a phenol) and one of its rings (the middle one) is a thiazine (which in turn is named for thio-, i.e. sulfur). It was originally used as an antipsychotic for its dopamine antagonist properties – in fact, it was the original ‘typical antipsychotic‘ that served as the template for a whole class of related drugs. It has largely (though not completely) fallen out of favor in psychiatric use as ‘atypical antipsychotics‘ (such as Zyprexa) have come into use. That it has fallen from favor is perhaps due to its horrifying side effects – as a dopamine antagonist it can cause Parkinsonian symptoms and sometimes irreversible tardive dyskinesia – though it is not clear that the newer antipsychotics are any better.
Korth 2001 was one of the original two papers that uncovered the in vitro efficacy of quinacrine against proteinase K (PK)-resistant PrPSc. This study also found chlorpromazine to be effective, though it was only a tenth as potent as quinacrine, having half-maximum effect at 3 μM compared to 0.3 μM for quinacrine. Meanwhile, at its most effective concentration, chlorpromazine was toxic enough to kill many of the cells, while quinacrine was effective at nontoxic doses. So right off the bat, chlorpromazine wasn’t as good a candidate as quinacrine was.
But unlike quinacrine, chlorpromazine had already been tested in scrapie-infected mice. Roikhel 1984 had tested chlorpromazine (referred to as ‘aminasine’) in scrapie-infected mice and found, oddly, that it prolonged incubation time in mice infected intracerebrally but not in mice infected intraperitoneally. There was earlier in vitro research as well: Dees 1985 had found that chlorpromazine plus ultraviolet irradiation could inactivate prions, though Dees incorrectly concluded that this was due to chlorpromazine’s nucleic acid-binding properties.
Barret 2003 followed up on Korth’s work by testing chlorpromazine, in addition to quinacrine and a few other compounds, in vitro and in scrapie-infected mice. In vitro, chlorpromazine did appear to reduce the formation of PK-resistant PrPSc. For the in vivo experiment, groups of 5 mice, infected intrapertioneally with 6PB1 prions, were treated with 10mg/kg/day quinacrine and/or 5 mg/kg/day chlorpromazine starting from 1 day post-infection. This wasn’t a survival study; the mice were sacrificed 30 days later to test the concentration of PK-resistant PrPSc in their spleens. Chlorpromazine had no effect on this metric, whether alone or in conjunction with quinacrine.
And that seems to be the full extent of in vitro and in vivo research on chlorpromazine as an antiprion. Trevitt & Collinge 2006, in a thorough systematic review of antiprion compounds explored up to that time, do not cite any additional studies of chlorpromazine beyond what I’ve just listed here.
As mentioned in the quinacrine post, UCSF began compassionate use of quinacrine and chlorpromazine almost immediately after the Korth paper was published, in August 2001. One of the patients they treated was a young British woman named Rachel Forber who had vCJD. Within a few weeks, the Times of London reported that Ms. Forber had improved massively and “enjoying a holiday with her father in Spain”. The Daily Mail, world’s most reputable newspaper, went even further, declaring that she had been cured. Unfortunately, BBC reported three months later that she passed away.
During those three months, Amaral & Kristiansen 2001 published a review arguing a possible mechanism for chlorpromazine’s efficacy based on Ms. Forber’s improvement, the in vitro evidence mentioned above, and a lengthy review of chlorpromazine’s efficacy in other unrelated disorders. (Korth 2001 was more cautious, stating that the mechanism was unknown).
Later attempts to treat patients with chlorpromazine weren’t any more successful. Benito-Leon 2004 treated two FFI patients with quinacrine and chlorpromazine. Neither patient’s condition improved, and one had an adverse reaction to chlorpromazine (orthostatic hypotension) so it had to be withdrawn. Benito-Leon, citing the animal studies that had already emerged by that time to show quinacrine was not effective in vivo, declared that it was time to give up on these two drugs for prion disease patients. Martinez-Lage 2005 reports on the use of combined quinacrine and chlorpromazine in a iatrogenic CJD case, again with no improvement.
And, at least as far as the literature shows, that was the last time any doctor prescribed chlorpromazine for prion disease. Rightly so. But that wasn’t the quite the end of the road for phenothiazines. This class of drugs featured prominently in hits from a high-throughput screen by Kociscko 2003. Chlorpromazine also provided the inspiration for the Wisniewski lab’s 2011 trial of fluphenazine, another phenothiazine typical antipsychotic, in scrapie-infected mice. That drug appeared possibly promising, with a 21% delay in onset versus controls, although the mice were infected peripherally and treated from 0 dpi, meaning there’s no evidence here that this would work against an infection already established in the CNS.
Of course, there is no doubt that phenothiazines cross the blood-brain barrier, given their long history as antipsychotics. It will be interesting if someone is able to show an effect for phenothiazoles in mice infected intracerebrally or carrying a genetic prion disease mutation. But even then, given the terrible side effect profile of this class of drugs, it would have to be a pretty large effect size for me to want to prioritize work on a phenothiazine over some of the more harmless drugs for which effects in prion-infected mice have already been demonstrated.