A brief history of prion propagation in cell culture
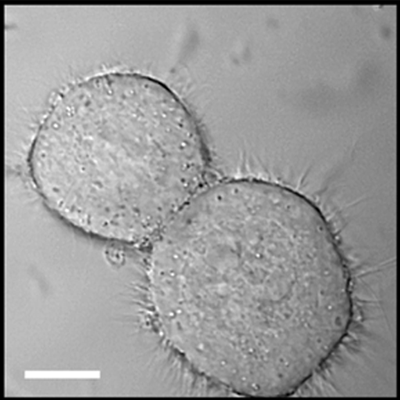
Above: N2a mouse neuroblastoma cells. From Wadia 2008 – Fig 1C.
prehistory
People have been trying to propagate the “scrapie agent” in cell cultures since at least 1970. The earliest study I found [Clarke & Haig 1970] does cite one earlier work but full text isn’t available online. The goal of Clarke & Haig’s study was to show that the “scrapie agent” could grow and replicate outside of the live animal. Then as now, the only way to know you’d generated infectivity was to inoculate the material into animals and see if they got sick. So Clarke & Haig took cells from the brain of a scrapie-infected mouse, grew them in culture, and then showed that they could infect other mice. But how do you know the infectivity was generated in cell culture and not just maintained from the original inoculum? They argued that they’d done enough serial passages of the cells to dilute the original infectious material by 10-7.8 thus removing “most” of the original infectivity.
It’s hard to follow the arc of literature from so many years ago, so I’m not sure what exactly became of this cell line or the others reported by the same group [Clarke & Millson 1976]. But not everyone was impressed. In his seminal prion paper [Prusiner 1982], Prusiner dismissed all prior efforts in a single sentence :
Attempts to propagate the scrapie agent in cell culture have been disappointing.
the advent of ScN2a
Prusiner then embarked on his own quest for a prion-infected cell line, finally succeeding a few years later [Butler 1988 (ft)], around the same time as another group [Race 1987, Race 1988]. The Butler study used N2a cells, a long-cultured mouse neuroblastoma cell line – in fact, George Carlson once told me that N2a cells have been cultured since before he was born. From what I see online that might be a slight exaggeration – the oldest study cited by the commercial provider of the cells, ATCC, [Olmsted 1970] says the cells were derived in 1967. Caughey used three mouse neuroblastoma cell lines designated DL, DK and C-1300. In any event, both Prusiner and Caughey took the approach not of deriving cells from prion-infected mice, but rather to drop infected brain homogenate on top of existing cell lines. Then they cloned the cells.
What cloning means in this context is as follows. You spread the cells into wells of a 96-well plate or similar at a dilution such that some wells will get exactly one cell. When you do this, the number of cells in each well end up following a Poisson distribution. So if λ is the mean density (cells per well), then the number of wells with k cells is given by:
.
The wells with exactly one cell are call monoclonal and the fraction of wells that are monoclonal is maximized at 1/e ≈ 37% when λ = 1. The math is exactly the same as trying to get monoclonal populations of DNA fragments onto a bead for next-gen sequencing, as mentioned in this post.
The reason you want monoclonal wells is that then you can culture cells in that well and know that they all came from the same parent cell, or in lab parlance, they’re all from the same clone. This means that they’re all genetically identical – at least until they mutate again (which for long-cultured tumor cell lines is not long). It’s also a good way to prove that any prion infectivity in the cells is new – generated in cell culture – and not just left over from the original brain homogenate.
Butler tried a variety of combinations of cell line and brain homogenate titer and found that only N2a cells infected at the highest titer of RML prions were able to sustain infectivity. In fact, of the 5 clones obtained from that batch of cells, only one clone (“clone 3″) turned out to be stably prion-infected [Butler 1988 (ft)]. Apparently they also obtained at least one clone infected with Fukuoka-1 prions, though they don’t go into as much detail on that.
Prusiner cast the development of these cells – dubbed ScN2a – as one more piece of evidence for the prion hypothesis [Butler 1988 (ft)]. Meanwhile, Caughey and Race were using their own scrapie-infected neuroblastoma cells for various experiments to characterize the cellular metabolism of PrP [Caughey 1989, Caughey & Raymond 1991], and after not long they started to help identify compounds that inhibited prion formation too [Caughey & Race 1992]. In time it appears that Caughey switched over to the ScN2a cells as well and adapted them for high-throughput screening [Kocisko 2003], a role they play to this day [Silber 2013].
But while ScN2a cells were proving themselves wildly useful, cell culture was also proving to be a source of profound frustration for scientists studying prions. It’s difficult to quantify that frustration from looking at published literature alone, because negative results are so rarely reported. But 25 years on, we still have no human equivalent of ScN2a cells, and even more frustratingly, we still have essentially no idea why.
more cell models, but no human prions
Later studies would extend the original basic procedure – infect, clone, bioassay – to obtain other combinations of prion strain + cell line. For instance, PC12 cells infected with ME7 or 139A prions [Rubenstein 1992] (which was weird since PC12 are rat cells while ME7 and 139A are mouse prions) or PrP-overexpressing N2a cells infected with RML, 22L and 139A [Nishida 2000]. Once pentosan polysulfate was discovered as a potent prion inhibitor, it could be used to cure ScN2a cells of their RML infection, whereupon they could be re-infected with 22F, 139A or 79A prions [Birkett 2001].
Over the years, prion-infected cell models have become a bit more diverse. For instance, mouse neurospheres were successfully infected with RML prions, representing a shift towards more of a stem cell model rather than a tumor cell line model [Giri 2006]. This is now the main cell culture model in use in George Carlson’s lab, for instance in their GPM6A work. Other investigators have managed to infect fibroblasts (as opposed to neuronal cell lines), originally by transfecting them to overexpress PrP [Vilette 2001] but later even without overexpression [Vorberg 2004b]. More recently, prions have been propagated in non-dividing myotubes (muscle fibers) [Herbst 2013]. The spectrum of species has broadened just slightly too, to include sheep prions [Vilette 2001].
Another /advance has been the ability to model neurodegeneration in vitro. N2a cells propagate prions, yet they don’t seem to suffer the consequences. This makes them useless for figuring out why prions kill. GT1 cells infected with RML, on the other hand, actually showed some signs neurodegeneration in vitro, which was a first [Schatzl 1997]. More recently, neurodegeneration has been observed in prion-infected cultured organotypic cerebellar slices [Falsig 2012], a model which has already been put to use deciphering mechanisms of prion neurotoxicity [Sonati 2013].
Yet despite all these advances, the prion infection of human cells has remained unattainable. One group reported that they had developed a human neuroblastoma cell line infected with CJD prions [Ladogana 1995], but this cell line was never to appear again in the literature, and eventually the authors admitted that it had “been lost” [see "Personal Communication" cited in Raymond 2006].
why not?
When people obtain positive (prion-infected) clones in their experiments, it is tough to say what makes those clones special. Take “clone 3″ from Butler’s original experiment – was it genetically different from its peers, or was it just the one cell that happened to get infected? It was shown that horizontal transmission of prions by cell-to-cell contact was possible [Kanu 2002] but later work would show that it was quantitatively quite rare [Ghaemmaghami 2007], with vertical transmission – mother cells to daughter cells – accounting for virtually all prion propagation, at least in ScN2a. So perhaps that one prion-positive clone was just “lucky”.
If “luck” is really the driving factor here, then the percentage of positive clones should correlate with the titer of the brain homogenate used to infect the cells. And indeed, higher titers do give a higher percentage of positive cells [Klohn 2003, Mahal 2007]. But that relationship between brain homogenate dilution and percent positive cells is different for different cell lines – some are more susceptible than others, by a lot [Bosque & Prusiner 2000]. Peter Klohn’s PK1 cells are a subclone of N2a which is > 1000x more susceptible than regular N2a cells, meaning they can be infected by a > 1000x weaker dilution of brain homogenate [Klohn 2003].
Long-cultured tumor cells tend to be genomically unstable, so it would be easy to imagine that some novel chromosomal rearrangement had rendered PK1 cells ultra-susceptible. Perhaps an important gene involved in some anti-prion pathway like alpha cleavage or autophagy had been knocked out by chromothripsis; perhaps a pro-prion gene had wound up under a stronger promoter and been overexpressed. The kinetics of prions in cell culture depend upon the balance between conversion, degradation and cell division [Ghaemmaghami 2007] so a change in any of these three rates could make the difference between a lot, a little or zero PrPSc accumulation. In support of this, it’s been found that many cell lines can be acutely infected with prions, but they clear the infection quickly such that only a few can be chronically infected [Vorberg 2004a].
If the issue was just that some cells were more susceptible to all prions than other cells were, a simple explanation having to do with, say, PrPSc degradation rates might be sufficient. But the strangest part of all is that susceptibility is strain-specific. R33 cells are highly susceptible to 22L prions but barely at all to RML; PK1 cells are susceptible to RML and 22L but completely resistant to infection by ME7 or 301C [Mahal 2007, see esp. see Fig 1]. Only CAD5 cells appear to be susceptible to a fairly wide range of prion strains.
The fact that such results have been replicated with different populations of cells grown from the same clone argues that there is something heritable about this strain specificity. I suspect that a lot of people have tried unsuccessfully to figure out what drives susceptibility, but very few have published their negative results. One study used karyotyping and aCGH to look for copy number differences associated with susceptibility, as well as qPCR on a few candidate genes to look for gene expression differences [Chasseigneaux 2008]. They didn’t find anything, which could be a lack of power or that there was nothing to find.
With 2013 technology we could do much better if we were willing to throw the resources at it – whole genome sequencing, jumping libraries to get chromosomal rearrangements at base pair resolution [Talkowski 2011], RNA-seq, and so on. ChIP-seq and bisulfite-seq to look for possible epigenetic explanations in histones or DNA methylation.
All that would be assuming that nucleic acids hold the key. But the hardest nut to crack will be if the phenomenon is epigenetic in a prion-like way. Meaning, maybe the conformation of PrPC or some co-factor differs between cell lines in a heritable, transmissible, evolvable way that determines susceptibility to different conformations of PrPSc.
The most interesting recent development in this area is that susceptible and non-susceptible cells are equally capable of supporting prion formation if they’re lysed and subjected to PMCA [Herva & Weissmann 2012]. That suggests the explanation is not as simple as gene expression or the straight presence or absence of a co-factor. The paper is entitled “Cell-specific susceptibility to prion strains is a property of the intact cell” but actually, I don’t think their results rule out an explanation relying on the conformation of PrPC or a co-factor. The sonication in PMCA disrupts conformation sufficiently to create de novo prions [Deleault 2007, Wang 2010] so surely it disrupts conformation enough to render hypothetical non-susceptible PrPC conformations susceptible to pre-existing PrPSc seeds.
At this point, I’ve wandered off into pure speculation. But there are some testable hypotheses here. If conformation is the issue, then could GdnHCl, shaking or sonication – all things that promote cell-free prion conversion – open up the conformational space to make cells infectable? Of course those things could kill cells too, so the question is whether there’s a “therapeutic window” where they might promote prion conversion without killing off the cells altogether. Or if conformation is not part of the equation, then the answer must likely lie in the cells’ genomes and we could figure it out with enough sequencing.
why prion-infected human cells would be a big deal
At this point it’s worth rewinding a bit to remind ourselves why we care. Prion-infected human cells would be a way to do high throughput screening (and followup experiments) on human prion strains, making it more likely we’d find drugs that work on human prions in vivo - as hits from mouse cell / mouse prion screens can turn out to be highly strain-specific. One approach to getting human prions into cell culture would be not to use human cells, but to express human PrP in N2a cells or similar. MRC Prion Unit has tried this, apparently with no luck so far (at least, I haven’t seen anything published).
So the mystery remains. At Prion2013, Stanley Prusiner opined that there was “something mystical” about infecting cultured cells with prions. We’ve gotten by so far with cell-free assays and in vivo assays, and if no one manages to infect human cells, we’ll probably continue to get by. But solving the mystery would be a big step forward – it would allow screening in human cells, and perhaps even more importantly, we might learn something fundamental about the nature of prion strains and how they replicate.