What gene therapy can and can't do today
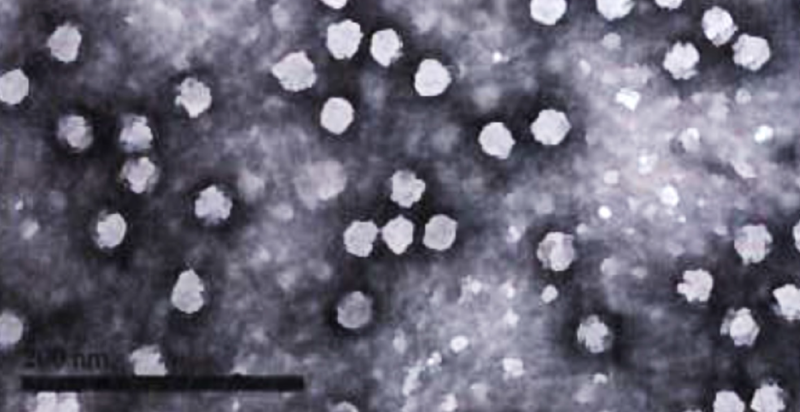
Electron micrograph of adeno-associated viruses (AAV), a type of viral vector often used in gene therapy. Reproduced from [Fuchs 2016] Figure S1.
Gene therapy is the source of a lot of real hope but also a lot of real hype. There’s no doubt that there has been progress and that there is more to come, but there is also a lot of confusion about what gene therapy can and can’t do as of today. As an example, one of the most common questions that Sonia and I get from family and friends and from members of our patient community is:
What about CRISPR? Now that we have the ability to edit genes, isn’t that your problem solved?
We strive to answer this question with the appropriate balance — new technologies including CRISPR are exciting and do present potential paths to therapy, but they’re also not our problem solved. Now, with the past two years seeing the first two FDA approvals of gene therapy drugs, I decided it was finally time to write a blog post about why gene therapy is exciting, but why it’s also not going to cure prion disease tomorrow.
In this post, first I will define what we mean by gene therapy. Then I’ll give an overview of the history and potential issues involved. I will spend most of the post going into three specific stories: of two newly approved gene therapy drugs and one tool developed in animal models that help to illustrate where the field stands today. Finally, I’ll conclude with some reflections on the prospects for a gene therapy for prion disease.
what is gene therapy?
Here, I’ll use the definition that gene therapy is the introduction or editing of genetic material in cells to treat a disease. This could include delivering a healthy, working copy of a gene to cells that are suffering from a loss-of-function disease, where they lack a working copy of that gene. Or it could include delivering a gene that will delete or interfere with a bad gene in cells suffering from a gain-of-function disease, for instance, using genes encoding CRISPR or RNAi constructs to turn off or turn down a disease-causing gene. Regardless, I am only including in this definition therapies designed to target somatic cells — cells in the adult body that are not involved in reproduction and where the gene therapy would not be inherited by future generations. I am not including here any discussion of germline gene editing.
My definition of gene therapy also does not include the antisense oligonucleotides (ASOs) that we are working on, nor does it include RNA interference (RNAi) therapies that have to be chronically dosed. We can call those things “genetically targeted therapies” because they are designed to target the RNA product of a specific gene, and we can call them “nucleic acid therapeutics”, since the drug itself is made of DNA, RNA, or similar. But they aren’t gene therapies because they don’t actually put new genes into cells. This is an important distinction both because of dosing — ASOs and the short interfering RNA (siRNA) used for RNA interference have to be dosed over and over, whereas once you’ve put a new gene into cells it could last for years or for life — and because of size — genes are thousands of bases long, and so encoding a whole gene takes a molecule thousands of times larger than an ASO or siRNA, on the order of megadaltons or larger, instead of kilodaltons.
Like many new technologies, the brief history of gene therapy [Wirth 2013] is one of lots of early hype, then sobering reality, and then (tentatively) a phase in which the technology matures and delivers on some of its promises, without as much of the hype. Studies of gene therapy first began in the late 1980s, and there followed a boom in which, as my mentor Stuart Schreiber likes to say, the “hype-to-hope ratio” was very high. That hype came crashing down in 1999 after a teenager, Jesse Gelsinger, died in a gene therapy trial after a severe immune reaction to the adenovirus used to package the gene. His death precipitated inquiries into oversight of gene therapy trials, and the late Jesse’s father testified to Congress about the need for tighter controls. After a long, sobering phase with little of either hype or hope, the gene therapy field has enjoyed a resurgence in recent years, where with a much more mature understanding of the constraints and safety concerns, people have started to be able to design safe and effective gene therapies and there are now two FDA-approved therapies. Still, there are many limitations and many open questions, so we still remain far from the future that some people imagined, even decades ago, in which every genetic disease could be treated with a gene therapy.
overview of how gene therapy works, and the challenges
Gene therapy is not, unfortunately, as simple as injecting genes into the bloodstream. Genes are made of thousands of bases of DNA, and these can’t get into cells on its own, so in order to put new pieces of DNA into cells in the body, you need to package that DNA in a virus. When I first heard this, I thought it was brilliant, the idea that we could hijack a virus to replicate throughout the body, infecting more and more cells and spreading a therapeutic gene as it goes. But it turns out it is not that simple either. For safety reasons, you don’t want to unleash a virus to go replicate on its own, so gene therapy only uses replication-incompetent viruses — either viruses that are naturally unable replicate on their own (because they normally rely on co-infection with other viruses), and/or have been engineered in the lab to be unable to replicate on their own. Such viruses can be produced in large quantities in the lab by growing them in cells that do have the genes necessary for virus replication, but those replication genes don’t get packaged into the viruses. Once they get into the body, each virus may be able to infect one cell, but it won’t be able to produce hundreds of progeny to infect hundreds of cells. Nonetheless, that one virus can plant its DNA in the cell, where it might stay for years or for a whole lifetime. Therefore gene therapy offers the enticing possibility of a single treatment to provide durable therapeutic activity.
While gene therapy studies have been conducted using a number of different viruses, by far the most common type of virus used in therapeutic development for neurological diseases is adeno-associated virus (AAV) [Deverman 2018]. AAV “in the wild” depends on co-infection with adenovirus. (Adenovirus was used in the trial in which Jesse Gelsinger died and, despite the similar name, is a whole different type of virus). On its own, AAV cannot replicate. Perhaps because AAV is pretty benign and does not cause any human disease, it is less immunogenic than many viruses, which makes it relatively safer to use for gene therapy. And while no naturally occurring viruses are highly efficient at getting directly from the blood into brain cells, some strains of AAV are relatively better at getting into the brain than most other viruses, which makes them more relevant for treating neurological disorders. A tradeoff is that AAV is small, a limitation I will touch on more below.
Gene therapy with viral vectors has appeared possible in theory for decades, and there are now two FDA-approved gene therapy drugs (see more below), but there are several practical issues and challenges that, taken together, form the answer to the question “why isn’t that your problem solved?”
Perhaps the foremost practical issue is delivery. How do you get the viruses into the cells that need them? There are 100 billion neurons in the adult human brain, and reaching enough of them is a tremendous challenge. Most approved drugs for brain diseases today are small molecules that can directly cross the blood-brain barrier and get everywhere in the brain, but viruses are far larger, and do not simply diffuse throughout the body. Some brain gene therapy trials have relied on direct injections of viral vectors into brain tissue, but viruses don’t diffuse throughout brain tissue either, so this approach generally only reaches a small focal region around the injection site. One company, Voyager Therapeutics, has ongoing and planned clinical trials to test whether this might be enough to make a difference in brain diseases where one brain substructure is disproportionately affected, such as the substantia nigra in Parkinson’s [Van Laar 2019] or the striatum in Huntington’s. We still don’t know the answer even in those diseases, and for a whole brain disease like prion disease, I do not harbor any hope that a focal delivery will be enough. Another possibility is intrathecal (IT) dosing into cerebrospinal fluid (CSF). The published data out there so far suggest that even with this delivery route, only 2% of the brain is reached in adult primates [Gray 2013], but a company called Avexis is planning trials to test whether they can do better than this (see below). CSF doesn’t touch all brain regions in equal measure, and so even if intrathecal delivery can be improved, it may not give an even brain distribution — for example, antisense drugs achieve some potency across the brain, but less in subcortex than in cortex. Every brain cell needs blood, however, and so one hope is that a systemic delivery through the bloodstream could ultimately reach more neurons than any other approach. But viruses will not simply diffuse from blood into brain, instead, they will only get into cells for which they have a specific “tropism”, usually meaning there is a specific receptor that the virus can grab onto in order to gain entry to the cell. Finding or developing viruses with a sufficient tropism for brain cells is a major challenge, and results from small animals like mice, or even from human infants, might not always translate to adult humans.
For many diseases, another major issue relates to cargo. What are you putting in your virus? For genetic diseases caused by a loss of function in an important gene, the main question is whether you can fit a healthy, functional copy of that gene into the viral vector you want to use. For genetic diseases caused by a gain of function, where we want to turn down or turn off a mutant gene, the main question is what you can put into your viral vector to shut down that target gene. There are a number of options here, which present various tradeoffs. A long-studied approach is to use RNAi, in which case the virus would produce an siRNA that targets the gene you want to turn off. Because you’re targeting the RNA, of which there may be many copies and they are produced constantly, you need your virus to keep producing its siRNA at high levels over years. Another approach is to have the virus encode CRISPR/Cas9, CRISPR-based base editors, or other genome editing systems. In this case even if the virus is only active at a low level for a short period of time, that may be enough to permanently edit the DNA in the cell. The flipside is that the CRISPR system might keep on editing the DNA in the cell for years and years, such that even if the therapy is deemed safe enough for human testing based on short term studies, one might accumulate many off-target edits throughout the genome over the years after receiving the drug, and this could eventually lead to a significant safety concern. Also, many CRISPR-based systems are too large to fit in an AAV. Yet a third approach, recently demonstrated in mouse models of Huntington’s disease [Zeitler 2019], is to use zinc finger repressors, which like CRISPR can be directed to a specific DNA sequence, but are designed to turn off transcription of RNA from the gene, rather than to edit the DNA. This approach still requires long-term activity of the virus to keep producing the zinc fingers, but compared to, say, the RNAi approach, the amount of zinc finger produced by the virus can be very low and still be effective, because each cell contains only two targets — the two copies of the gene — that need to be turned off.
Overlaid on both of the above issues are questions of safety and immunogenicity. While viral vectors used for gene therapy are replication-incompetent, they are still viruses, so many people will either already have immunity against them, or, there is a risk they could develop an immune reaction to the virus upon receiving the therapy. As noted above, AAV are relatively low-immunogenic, but that still doesn’t mean this problem goes away. The engineering of AAVs that are less immunogenic, or that people simply have not yet been exposed to, is an area of active research [Zinn 2015]. There are also issues with the potential immunogenicity of the cargo being delivered. For example, Cas9 is a bacterial protein, and has never been injected into humans in a therapeutic setting. It is possible that people will turn out to have, or develop, immunity against Cas9. A quick search for CRISPR on ClinicalTrials.gov revealed that all ongoing trials are ex vivo, meaning that cells are taken out of the body, edited with CRISPR, and then put back. To my knowledge, Cas9 has never actually been put into humans before, so its safety and immunogenicity profiles are not yet known. This is one reason why some scientists I have spoken with believe the zinc finger approach is closer to in vivo human gene therapy applications than CRISPR. While a specific zinc finger protein engineered for any one disease, such as Huntington’s, may be novel, humans already naturally have many zinc finger proteins that are similar, so the risk of immunogenicity may be lower. Of course, as with any drug, viral vectors can also have variety of potential safety concerns, not limited to immunogenicity. For example, for any specific cargo you may worry about off-target effects — for example, does your RNAi against your target gene also lower the RNA for some other, very important, gene? And while AAV DNA stays by itself (“episomal”) once it is in the cell, certain other viruses that have been investigated for gene therapy, such as lentivirus (a modified form of HIV), can integrate into people’s DNA, and might happen to turn on an oncogene and cause cancer. Finally, even though viral vectors are engineered to be replication-incompetent, another risk is that, perhaps by random mutation or by co-infecting the same cell as another virus you encounter “in the wild”, they might manage to become replication-competent once they are in a human.
Gene therapy is an area of very active research, and there are scientists hard at work on trying to overcome all of the various obstacles I just described. Already we are seeing some breakthroughs, where for some diseases in some tissues some of the time, gene therapy actually works. At the same time, hopefully the above obstacles give a sense of why our problem is not solved yet. To give a better sense of how far we’ve come and how far we have yet to go, in the next three sections of this post I will review the two FDA-approved gene therapies, and one breakthrough in viral vectors for mouse studies, before concluding with some thoughts on the potential for gene therapy in prion disease.
gene therapy for inherited blindness
In December 2017 voretigene neparvovec-rzyl (Luxturna®, developed by Spark Therapeutics), became first-ever FDA-approved gene therapy. It is an AAV2 vector engineered to express a working copy of the gene RPE65, injected into the retina to treat blindness in people who lack a working copy of that gene. The approved dosing regimen is as a one-time therapy, with a dose of 1.5 × 1011 viral genomes (vg) injected in a volume of just 0.3 mL, in each eye.
The road to voretigene was 20 years in the making. As soon as it was discovered that homozygous loss-of-function mutations in RPE65 cause inherited blindness (with phenotypes known as Leber’s congenital amauropathy and retinal dystrophy) [Gu 1997, Marlhens 1997], it was recognized that two factors would make this a prime candidate for viral vector gene therapy. First, the compact size of the gene would make it feasible to deliver in an AAV — the virus’s carrying capacity is just 4.4kb of DNA, too small for some human disease genes but plenty large enough for RPE65. Second, the retinal photoreceptors affected in this disease comprise a compact enough tissue that efficient delivery of enough virus to the affected cells might be feasible. Within just a few years, an AAV expressing RPE65 showed efficacy in a dog model of the disease — an incredbile turnaround from gene discovery to preclinical proof-of-concept for a therapeutic strategy [Acland 2001]. Within a few more years, multiple different groups worldwide had begun human studies of AAVs expressing RPE65 [Bainbridge 2008, Maguire & High 2009]. Because these trials all relied on just a single dose (per eye), patients were followed over ever-longer periods to evaluate their visual trajectory and determine how long the virus remained active [Cideciyan 2009, Jacobson 2012, Le Meur 2018]. A phase III trial finally showed clear evidence of efficacy for one of the vectors [Russell 2017], and the drug was approved.
Out of all the gene therapies that have been in development for various diseases over these past 20 years, voretigene was the first approval, and so counts as an outstanding success. But it is important to realize that behind that success there were still a lot of hiccups, twists and turns, and failures. For example, it was recognized that in order for the therapy to work, patients would need to still have retinal photoreceptors left for the virus to transduce, and it was found that while younger patients had photoreceptor impairment, more advanced patients had photoreceptor layer thinning consistent with cell loss [Jacobson 2005]. This may have been why trials excluded patients who were too advanced [Russell 2017]. And voretigene (developed by Spark Therapeutics) was not the only RPE65 AAV under commercial development — searching on ClinicalTrials.gov I found at least two very similar products for which development was eventually discontinued: one by AGTC [Pennesi 2018] and one by Targeted Genetics Corporation [Stieger 2010]. Why did these therapies, which were the same gene in essentially the same virus, stall out where voretigene succeeded? One eye gene therapy researcher I spoke with speculated that the most arcane details of drug preparation and deilvery may have made the difference. She suspected that in one trial, too much of the viral dose had been lost when it stuck to the inside of the plastic catheter used to deliver the dose into the eye. To me, this possibility was eerily reminiscent of our finding that plastic exposure can be a major determinant of PrP concentration in cerebrospinal fluid if samples are not handled with exquisite uniformity [Vallabh 2019]. It’s yet another reminder that no matter how clear the therapeutic hypothesis, getting all the details to align correctly to develop a drug is never trivial.
For patients with RPE65 mutations, voretigene seems to be making a huge difference in their quality of life. What does this drug mean for the rest of us? Given that the virus is delivered by a focal injection into the retina, it doesn’t tell us much about the feasibility of viral vector gene therapy for larger tissues. And given that the virus is intended to deliver a working copy of a broken human gene, it also doesn’t tell us too much about the path forward for gene therapies designed to turn down or turn off expression of a toxic mutant gene. But voretigene does teach us a lot that’s broadly relevant. With the caveat that the eye is relatively “immune-privileged”, voretigene helped to establish the tolerability of AAV gene therapy in humans, overturning longstanding fears that the immunogenicity of viral vectors doomed them to never become safe and effective drugs. Voretigene also demonstrated the long-term durability of AAV gene therapy, with efficacy maintained for at least 3 years [Jacobson 2012] and probably longer. Finally, while the details are obscure to me as I am not a viral vector expert, I am guessing that the pharmaceutical companies and scientists involved in making voretigene (as well as its discontinued competitors) learned a ton about how to design, manufacture, QC, store, and deliver viral vectors — none of which sounds like big science but all of which is difficult, and critical to get right.
gene therapy for spinal muscular atrophy
Two years after voretigene, we saw the first FDA approval of a viral vector gene therapy delivered not locally but systemically — throughout the circulation. The drug is called onasemnogene abeparvovec-xioi (Zolgensma®, developed by AveXis) and it is an AAV9 engineered to deliver a working copy of the gene SMN1 to children under age 2 with spinal muscular atrophy (SMA) caused by a lack of functional SMN1. Per the label, the drug is intended as a one-time dose of 1.1 × 1014 vg per kg of body weight (so about 400 trillion vg for a typical infant), infused into the bloodstream.
As with any drug development project, the road to here was long. A decade ago, mouse studies of systemic delivery of AAV9 expressing green fluorescent protein, useful to track where the virus goes, provided a hint that AAV9 might be useful in SMA [Foust 2009]. In neonates (1-day old animals), systemic delivery of AAV9 resulted in a good amount of virus uptake throughout the brain, but especially in spinal cord motor neurons. In adult mice, the systemic delivery did not do nearly as good a job of reaching motor neurons, with brain distribution instead restricted mostly to astrocytes. But SMA, in its most severe form, is an infantile-onset disease where motor neurons in the spinal cord are the principally affected cell. Therefore, there might be an opportunity for AAV9 to treat SMA. Sure enough, preclinical studies in mice [Foust 2010, Bevan 2011] and then pigs [Duque 2015] provided strong evidence that AAV9 could indeed deliver SMN1 to the motor neurons that needed it. In the open label human trial, all 15 infants treated with onasemnogene were alive at age 20 months [Mendell 2017], a survival rate nearly unheard-of in untread historical control cohorts [Finkel 2014]. After the antisense oligonucleotide nusinersen, onasemnogene became the second approved targeted therapy for SMA. In a neurodegenerative disease that was essentially untreatable a few years ago, to now have two effective drugs is an incredible turn of fortunes, and a reminder of why, even when science is slow and frustrating in the short term, there are reasons for great optimism in the long term.
In concrete terms, what does onasemnogene mean for the rest of us? The fact that it is delivered systemically, as opposed to voretigene which is delivered into the retina, is a huge leap forward. This shows us that systemic delivery of a huge amount of virus can be tolerated without an immune reaction, and can reach disease-relevant CNS tissues. In other words, it provides key data on tolerability and reach. But there are caveats to both of these points.
The major caveat to tolerability is the issue of seropositivity: many people have been exposed to AAV9 or a similar AAV serotype in their daily life and have immunity against it, meaning they have circulating antibodies against the virus. In order to enroll in the onasemnogene clinical trial, patients had to be seronegative for (not have antibodies against) AAV9. Only 1 out of 16 infants failed that test [Mendell 2017], but one study estimated that the rate of AAV9 seropositivity in adults is as high as 47% [Boutin 2010], although this included adults with a pretty low titer of antibodies. Would an AAV9-based gene therapy be safe and effective in seropositive people? We don’t know yet. The FDA-approved label for onasemnogene abeparvovec recommends that doctors order AAV9 seropositivity testing before administering the drug, and cautions that “The safety and efficacy of ZOLGENSMA in patients with anti-AAV9 antibody titers above 1:50 have not been evaluated,” although it does not prohibit doctors from prescribing the drug to seropositive patients anyway.
The major caveat regarding reach is that the onasemnogene trial was conducted on babies — the oldest patient in the trial was 8 months old [Mendell 2017]. So this has to be viewed in the context that the mouse data suggested ten years ago that systemic AAV9 did a great job of reaching motor neurons in babies and not such a good job in adults [Foust 2009]. Could an AAV9 gene therapy reach enough disease-relevant neurons to modify disease in an adult human? This question is still live. Avexis, the company that developed onasemnogene, now has a clinical trial (called STRONG) for slightly older SMA children using intrathecal instead of systemic delivery of the drug, and according to their press release the data presented at the AAN2019 conference showed improvement in motor function in all 12/12 children in the older age group — but this is still only ages 2-5. Avexis’s pipeline shows a gene therapy for SOD1 ALS — a motor neuron disease of adults — now in preclinical development, and an abstract presented at AAN2019 [Thomsen 2019] says they found “efficient transduction and SOD1 downregulation throughout the entire CNS” in 3-4 year old monkeys and one 10 year old monkey. That sounds highly promising, and clinical trials, which are apparently now being planned, will provide an important test of the relevance of AAV9 therapy for adult CNS disorders, albeit with the caveat that SOD1 ALS still predominantly affects spinal cord motor neurons, whereas a whole brain disease like prion disease might be a harder beast still.
development of better AAVs
The AAV9 data discussed above lead to the question: what can we do to get better virus uptake in the brain cells we care about? It is possible that intrathecal delivery, meaning injection into the cerebrospinal fluid, might do better than systemic delivery, although it probably won’t be perfect either. Not all CNS tissues are in equal contact with cerebrospinal fluid, and intrathecal ASOs, for example, achieve broad brain distribution but with relatively better potency in cortex and relatively less potency in subcortex, so it is possible the same will turn out to be true for intrathecally delivered viruses. It is also possible that simply upping the dose — injecting more viral genomes systemically — could help reach more brain cells, though it’s an open question whether one would eventually hit some limit where the large dose triggers an immune reaction or some other dose-limiting safety concern. A third possibility is to engineer viral vectors with superior tropism, that are more specifically taken up by the cells of interest.
On the topic of engineering better viral vectors for reaching the brain, a fascinating development over the last few years has been the story of the AAV PHP.B and AAV PHP.eB vectors (sometimes referred to as the “Caltech AAV”). Researchers started with AAV9, and set out to find a better, more brain-tropic vector, using a series of clever genetic tools to, first, generate genetic diversity in the AAV capsid (by randomizing a seven amino acid sequence exposed on the virus’s surface) and, second, select those viral genomes thad had gotten into the brain (by injecting the virus into transgenic mice that expressed a Cre switch allowing selective recovery of only those viruses that had gotten into certain pre-determined cell populations). They came up with a vector called PHP.B, with about 40-fold higher brain uptake than AAV9 [Deverman 2016]. They then repeated the same trick, but with PHP.B as a starting point, generating diversity in additional amino acids, and using various transgenic mouse lines allowing selection of viruses in astrocytes or specific neuronal populations. This resulted in an even better vector, called PHP.eB, with about twice the brain uptake of the original PHP.B [Chan 2017]. In adult mice given a 1 × 1011 vg systemic dose of PHP.eB, 69% of neurons in the cortex and 55% in the striatum (a region of subcortex) were reached. That’s well within the range where you could imagine making a big impact on many neuronal diseases.
After PHP.eB was made widely available to the research community, multiple groups undertaking mouse experiments came to recognize that PHP.eB’s brain uptake differed a lot between mouse strains. In C57BL/6 (“black six”) mice, the strain in which PHP.eB was discovered, brain uptake was excellent, but in BALB/cJ mice, it was no better than the original AAV9 [Hordeaux 2018]. The group that had developed PHP.eB set out to identify the virus’s receptor, using the clever and, to my knowledge basically unprecedented, approach of a genome-wide association study between different inbred mouse strains [Huang 2019]. They tested the brain uptake of PHP.eB in 13 different mouse strains, and found 7 strains with good uptake and 6 with poor uptake. These mouse strains had already been sequenced in the Mouse Genome Project, so the genetic data were already there — all that remained was to see which genetic variants correlated with virus uptake. Running the genome-wide association study using Hail narrowed the field down to two related genes, both of which were expressed in the brain endothelial cells that comprise the blood-brain barrier, and one of which, Ly6a, was already known to be associated to mouse susceptibility to several other viruses. CRISPR editing experiments confirmed that Ly6a was the receptor, and analysis of its sequence across mouse lines suggested that the key difference was a whether the gene’s protein product was GPI-anchored or not — mouse strains with an amino acid sequence predicted to result in GPI anchoring had good virus uptake, and those with a mutation that disrupted GPI anchoring had poor virus uptake.
The bummer is, it turns out that you and I don’t even have Ly6a — this mouse gene simply has no ortholog in humans, whether GPI-anchored or not. Although no one has tested it, PHP.eB would be expected to have no better brain uptake in humans than AAV9 does. But while this whole story hasn’t yet resulted in a viral vector poised to cure human brain diseases, there are a few reasons to think that it represents a major step forward. First, the researchers established a method that succeeded in generating a vastly improved viral vector. That method, or variations on it, may yet yield vectors that bind a receptor that we humans do have. Second, the ability to swiftly identify the receptor of an improved viral vector is a crucial advance that might be applied to figuring out whether new vectors discovered in the future could be useful in humans, and it is even possible that Ly6a itself gives us some hints about the properties that a good receptor needs to have. Third, although broad and efficient delivery to the adult human brain is a principal challenge in gene therapy today, it isn’t the only challenge, and PHP.eB will likely serve as a tool to help us to solve some of the other challenges. Used in proof-of-concept experiments in mice, PHP.eB could help us sort out questions like how much gene delivery or how much knockdown, in which cell types, achieved through what mechanisms, is necessary for efficacy in various brain diseases.
conclusions: where we are and where we need to go
I titled this post “what gene therapy can and can’t do today,” but really, the question is between what it can do, and what it hasn’t yet been shown to do or we haven’t yet figured out how to do.
In terms of delivery, gene therapy can reach a small piece of tissue through targeted injection, or can reach a fairly broad swath of the brain after systemic injection in infants. We don’t yet know if/how it can reach a broad swath of the brain in older children or adults. Trials that are either underway or in the works may tell us whether intrathecal delivery, or simply using an enormous dose of virus, can reach a meaningful percentage of brain cells in adults. If the answer is yes, fantastic, but even if the answer turns out to be no for AAV9, the engineering of better viral vectors, as illustrated by the PHP.eB story, may offer a solution.
In terms of safety, gene therapy with AAVs, even systemically, seems to be well-tolerated in seronegative individuals. We still don’t know whether these therapies will be safe and effective in seropositive individuals, or whether it might be possible to temporarily dampen immune response enough to allow these individuals to benefit. And the existing data speak mostly to the tolerability of the AAV itself. There are still many open questions about the immunogenicity of different cargoes you might want to package into an AAV, such as whether people will have a reaction to the bacterial Cas9 protein used in CRISPR systems.
In terms of durability, data now suggest that AAVs stick around for at least a few years, and probably longer. There is no indication yet from any of the ongoing trials that efficacy falls off after a certain amount of time, and currently approved therapies are being framed as a single dose for a lifetime. Whether efficacy truly persists for decades remains to be proven, but at a minimum, the dosing regimens for AAV therapies are likely to be far less frequent than for any other therapeutic modality.
In terms of cargo, all of the gene therapy advances discussed here — the two approved drugs and the vector engineering efforts — center on AAV, whose 4.4kb capacity is enough for replacement of many genes, including RPE65 and SMN1, but not others, such as the gargantuan DMD. For treating gain-of-function diseases, AAV’s capacity is enough to deliver RNAi or zinc finger repressors, but not enough for many CRISPR-based systems. Delivery of larger cargoes will either require engineering multiple AAVs to encode separate pieces of a gene or complex, which due to combinatorics will only work with very high delivery efficiency, or will require different vectors altogether. While not everything fits, there are a large number of genetic diseases (including prion disease) that could be treated with the existing capacity of a single AAV vector.
Where does all this put us? My mission in life is to develop a drug to prevent prion disease, which is an adult onset disease of the whole brain, where we would need to substantially lower PrP expression in essentially all brain neurons to really put a stop to the disease process. Could this be done with gene therapy? We are not there yet. There are a lot more unanswered questions about gene therapy for this type of disease than there are for antisense oligonucleotides (ASOs), which is why we are pushing full force to get ASOs against PrP into the clinic as soon as we possibly can. But gene therapy for prion disease no longer sounds like science fiction either. The SOD1 ALS gene therapy trials that are now being planned may answer the question of whether, with the right dose and right delivery route, existing AAV9 vectors might actually turn out to have enough brain uptake to make at least some difference in adult CNS diseases. Based on the available published data to date, it appears likely that we will need better vectors than existing AAV9 for a whole brain disease like prion disease. But even if so, there is hope that engineered vectors optimized for brain uptake might get us there in the next several years. Therefore, it may not be premature to be considering proof-of-concept experiments in mice, to answer questions about what gene therapy approach would make sense if and when we have the right vector. For example, what cargo would we want to put into an AAV to treat prion disease, how potent would that cargo need to be, what brain distribution would we need to achieve, and when in disease could we treat? Answering these questions for prion disease will increase the chances that, when the viral vectors become ready, they can be swiftly and effectively deployed against our disease.